Check out more of our Shots videos!
and live on Freeview channel 276
Visit Shots! Now
Specialists at Northampton General Hospital are using a 3D printer to create specialist masks to fight skin cancer without the need for surgery.
In 2021, the hospital introduced cutaneous brachytherapy – a highly targeted radiation therapy technique used to treat certain types of basal cell or squamous cell carcinoma of the skin.
The treatments are carefully tailored to the patient and – because the surrounding healthy tissue is spared from radiation – can be used instead of surgery and lead to a faster recovery with good cosmetic results.
 LR Dr. Deepali Vaidya, Susan Galloway, Bansi Mulji-Shah and Maulik Darji.
LR Dr. Deepali Vaidya, Susan Galloway, Bansi Mulji-Shah and Maulik Darji.
Last month (January), the hospital used a highly specialized 3D printer for the first time to create a custom face mask for a patient with skin cancer on her nose that would otherwise have required surgery and likely plastic surgery.
Bansi Mulji-Shah, head of the Service Improvement Skin project, said: “We used the 3D printer to print a customized face shape for this patient and treated the skin with brachytherapy (a form of radiotherapy).”
“Due to the shape of the skin cancer on the patient’s nose, it would have been very difficult to treat her cancer using traditional methods of radiotherapy. The alternative would have been to offer the patient an operation that would have involved extensive cosmetic changes, which the patient would have refused.
“With this new tailored method using the 3D printer, we are able to treat her cancer with radiation therapy without the extensive cosmetic side effects.

 Ms Galloway receiving treatment with the tailor-made mask
Ms Galloway receiving treatment with the tailor-made mask
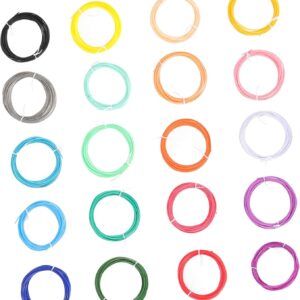
“With special thanks to our physics team (Stuart Duggleby, Stuart Tomlinson, Ahmar Yaseen and Steven Stibbs), the printer essentially creates a plastic mask filled with tissue-like material. The mask is printed with millimeter-sized tube holes that we used to direct radiation to specific points and in depth and precisely to the part of the skin where the cancer is with sub-millimeter precision.
“A series of treatments destroy the skin cancer cells without the need for an invasive cut into the skin.”
NGH’s clinical oncologist, Dr. Deepali Vaidya, said: “Squamous cell carcinoma and basal cell carcinoma are the most common types of skin cancer, affecting around 1,000 people in Northamptonshire each year.
“They are highly curable – and less dangerous than melanomas – but can be disfiguring and costly to treat and require surgery or other forms of more extensive radiation therapy.”
“The new treatment is a better option for many patients and the use of the 3D printer mask helps us to target it very precisely, especially for patients with skin cancer with difficult shapes or in difficult locations.”
“It is also a better treatment option for older patients who do not heal as well, or for patients with cancers of the nose, ear or eyelid who may require multiple surgeries to achieve a comparable treatment result.”
The first patient is satisfied with the simplicity and precision of the new treatment
The first patient to receive the new treatment was Susan Galloway, 76, from Duston, Northampton.
She was diagnosed with skin cancer on her nose last year and agreed to radiation therapy using the new 3D printer mask in January.
Ms Galloway, who is widowed and has three children and eight grandchildren, said: “They took some very precise measurements and fitted me the mask.
“I received eight treatments starting on January 16th and completing on January 26th.
“From start to finish, each treatment took about 20 minutes and I had to grab a tube with my teeth, which was a bit awkward, but okay. Afterwards you will feel the effects of radiation therapy and your nose will hurt a little, but the skin cancer cells will be killed, which is what you want.
“I think if you need this kind of treatment, you should get it. There is little inconvenience and you can get rid of your cancer.”
Ms. Galloway had a follow-up appointment and is doing well.
NGH is currently working to expand the service using 3D printers to develop customized applicators for more complex and advanced skin cancers.
The aim is to raise awareness of this treatment option among both local health professionals and patients about its availability.